
Scaling Up and Transforming Health Workforce Education and Training for Improved Health Equity
This post was originally published on the Global Health Workforce Alliance Members’ Platform. We encourage you to join and contribute to discussions like this one.
The statistics are startling: today the world is in urgent need of 7.2 million additional doctors, nurses, and midwives, according to the WHO, and by 2035 that number will rise to 12.9 million. Recent estimates show that just under one million doctors, nurses, and midwives graduate each year. At this rate, it would take more than seven years to produce the additional skilled workers currently needed. Yet in seven years, the need for health workers will be much higher.
Scaling up and transforming the health workforce for increased health equity is not simply a question of producing more of the same health workers. Key stakeholders and decision-makers in the education and health sectors face three important barriers to developing an effective, accessible, and sustainable workforce:
1. Maldistribution of health workers, both geographically and within health systems
The health workforce tends to concentrate in urban areas, higher-income countries, and tertiary care facilities, leaving populations and geographical areas with the highest burden of disease and the fewest resources with the largest deficit of health workers.
2. Poorly connected and aligned education and training institutions
Education systems must address some of the systemic failures identified by the Global Commission on Education of Health Professionals for the 21st Century. In addition to limited production capacity, these include mismatches between competencies being developed and actual health needs, weak preparation of graduates to work in health care delivery teams, gender stratification, hospital-dominant training, and the proliferation of professional silos.
3. Limited investment in education
Worldwide, less than 2% of health spending is dedicated to educating the next generation of health workers. Clearly there is a need for increased investment, as well as a need to use existing resources in the most efficient and effective ways.
The USAID- and PEPFAR-funded CapacityPlus project has partnered with international, regional, and national stakeholders in education and health to support education systems in producing more health workers who are not only competent and qualified, but also relevant to local needs. As part of this work, CapacityPlus has developed a number of approaches and tools:
School Management Package
Through no fault of their own, senior leaders of health professional schools and associated clinical practice sites frequently have little management training and are unaware of inefficiencies that may occur within their facilities. CapacityPlus’s School Management Package considers nine dimensions of management (see figure below), all of which support any school’s educational mission, vision, and goals. The package aims to identify management challenges at an institution, set goals, and guide leadership in applying good management practices. Currently at the end of its pilot phase, the package will consist of a self-assessment tool, prioritization and planning tools, a selection of management tools, and the Dean’s Dashboard, a free, open source software program intended to assist in managing data essential to running a school and tracking schools’ progress toward management improvement goals.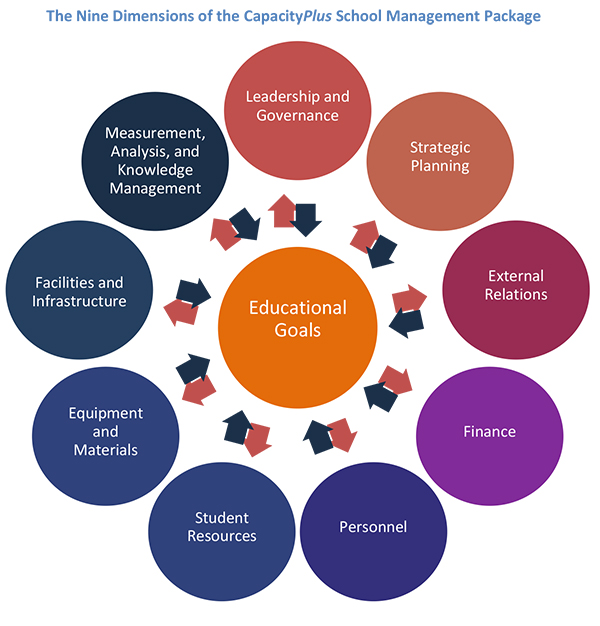
Bottlenecks and Best Buys approach
Already used at more than 50 schools of nursing, midwifery, community health, and medicine in seven countries, the CapacityPlus Bottlenecks and Best Buys approach is a comprehensive way to discover what cost-effective actions can be taken to produce more competent and qualified graduates. Bottlenecks assessments consider issues ranging from student and educator retention through the importance of partnering with other institutions for high-quality outcomes. After leaders discover bottlenecks impeding their progress toward these goals, the “best buys” component assists in identifying and costing actions that can have large impact at minimal costs.
Costing methodology
In partnership with the US Government’s Nursing Education Partnership Initiative (NEPI), CapacityPlus developed a method for estimating the “unit cost” to an institution and its affiliated clinical sites to produce a single graduate. The approach allows planners and policy-makers to consider the cost of educating a single worker as well as the effect a planned change in a program would have on the per-graduate cost of education (for instance, implementation of a community-based educational rotation). Using this methodology, a pilot study was completed at Walter Sisulu University in South Africa to estimate the cost of a five-year Bachelor of Medicine and Surgery program. Another study is under way in Ethiopia, in partnership with NEPI to estimate the costs of Bachelor of Science and Diploma nursing and midwifery programs at two colleges of health sciences.
Overcoming gender barriers
In Strengthening the Health Worker Pipeline through Gender-Transformative Strategies, CapacityPlus identifies issues that challenge women’s inclusion in the health workforce and recommends good practices to overcome them. Some recommendations are that schools implement sexual harassment policies, including a single code of conduct for students, faculty and staff; commit to policies that don’t require pregnant students to terminate their studies; allow pregnancy/maternity and parental leave for students and faculty; provide child care financial assistance; and permit students to learn with flexible course schedules. Here, a health worker in Namibia shares how she struggles to balance professional and family responsibilities.
In-service training and continuing professional development
Epidemiological, demographic, and technological changes are impacting what health workers must know. Learners in preservice education programs must receive the best, most up-to-date information possible. Moreover, after those learners graduate, they must have access to continuing education and training. That training must be routinely evaluated and revised to ensure health workers’ competencies are aligned with real needs. Based on a literature review, in-service training is most effective if there is a clear need for a particular activity, and learning is based on that identified need; if follow-up provision is made to reinforce lessons learned in training courses and link them to the health workers’ practice; and if in-service training is linked to preservice education, providing as far as possible a seamless continual professional development system. After surveying many PEPFAR-funded partners implementing in-service training programs in Nigeria, CapacityPlus recommended ways in which in-service training could be more efficiently utilized.
Questions for discussion:
- What is needed to engage key actors in the health and education sectors in the process of transforming health workforce education and training?
- What should be done to attract higher levels of investment in health workforce education and training?
- What are the measures or indicators of success for scaling up and transforming health workforce education for improved health equity?
Help CapacityPlus spread the word about strengthening the health workforce. Follow us on Twitter and like us on Facebook.
Related items:


