
Social Justice and the Global Health Workforce
 This year's American Public Health Association (APHA) annual meeting, themed around social justice, represented a strong commitment to addressing domestic and global health challenges, milestones, and successes. As Dr. Howard Koh, the United States assistant secretary for health, said, “If you don’t stand for something, you’ll fall for anything.”
This year's American Public Health Association (APHA) annual meeting, themed around social justice, represented a strong commitment to addressing domestic and global health challenges, milestones, and successes. As Dr. Howard Koh, the United States assistant secretary for health, said, “If you don’t stand for something, you’ll fall for anything.”
Energized participants and presenters expressed the importance of social justice, human rights, and the intersections in public health. It has been over 100 years since the APHA annual meeting was last held in Denver, and the Mile High City did not disappoint as this year’s host.
Health workforce constraints
Many presentations noted that health worker shortages are impeding success in improving global health. As Joan Cioffi from the Centers for Disease Control and Prevention noted, “The science is terrific, but no programs will get done without people.”
This interesting session focused on health workers’ rights in conflict and postconflict settings, and how as health systems and infrastructure are destroyed, health workers face limited support and sporadic aid from various developmental and political institutions. Exacerbating the challenges in rebuilding health systems in postconflict settings is the fact that health professional schools are also destroyed, limiting training opportunities for health workers.
Mental health services
Mental health services came up frequently in this session and, in particular, the lack of training in this service delivery area. In conflict and postconflict settings, populations are suffering from depression, posttraumatic stress disorder, substance abuse, and other mental illnesses that are rarely addressed. One panelist noted that rates of mental health disorders tend to double after emergencies, and shortages of psychiatrists, psychiatric nurses, psychologists, and social workers are barriers to addressing these problems.
Integrating this training into primary health care and using psychiatric nurses and mental health paraprofessionals may address some of these gaps. Using the life cycle approach for professionalizing under-recognized cadres, health professional schools and governments need to find ways to fill this gap in human resources for health.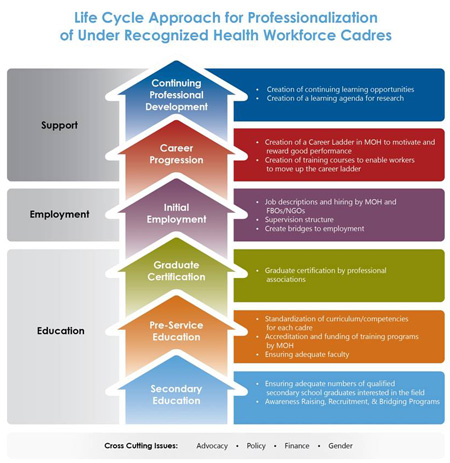 The life cycle approach
The life cycle approach
CapacityPlus is also using the life cycle approach to address under-recognized cadres—such as supply chain managers and social workers. This systematic approach can be applied at any stage of a health professional’s career. The phases include secondary education, preservice education, graduate certification, initial employment, career progression, and continuing professional development. By implementing the life cycle approach, these professional health cadres can establish career paths, better collaborate with ministries of health and professional associations, and ultimately better serve clients through an improved professional agenda.
Human rights, health worker rights
The APHA conference helped me to reaffirm my stance on the human right to health care access, which includes a trained health workforce. Likewise, I believe in the rights of health workers and their rights to receive high-quality training, and be respected and supported.
Image of life cycle approach courtesy of Kate Tulenko


